
Adverse Event reporting information can be found in footer
Request a Meeting
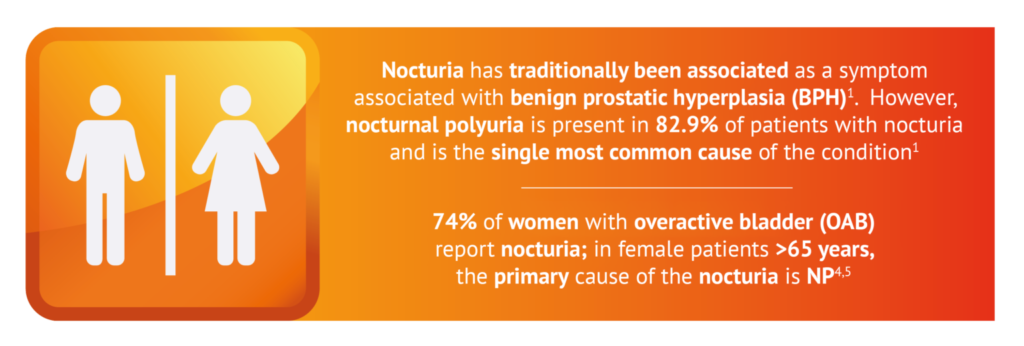
Nocturia has been traditionally regarded by urologists as a urine storage symptom associated with benign prostatic hyperplasia (BPH) and/or overactive bladder (OAB).1 BPH can result in bladder outlet obstruction (BOO) causing nocturia symptoms.1 Studies show that NP presents in 76-88% of reported nocturia cases -the majority of patients suffering from nocturia.1 More importantly, patients who suffer from OAB or BOO with persistent nocturia despite treatment may have underlying nocturnal polyuria as well.1 These findings are consistent regardless of gender, age, ethnicity and/or country;1 this discovery suggests NP can have its own pathology.1 A fuller understanding of the underlying causes of nocturia and correct diagnosis of patients suffering from nocturnal polyuria will help clinicians provide better patient care.
1. Increased nocturnal urine production
2. Reduced urine volume
3. Increased 24-hour urine volume
These three pathways can lead to nocturia symptoms via different mechanisms6
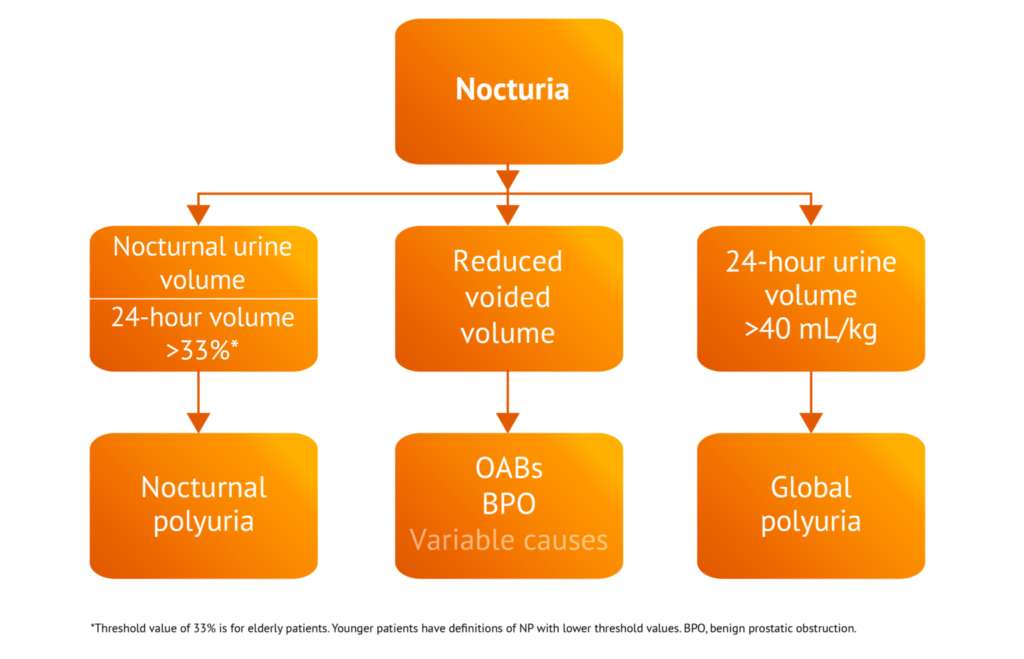
Adapted from: Van Karrebroeck of al. Neurourol Urodyn 2002;21:179-183.6 Copyright © 2002.
For more information, download our differentiation guide for further guidance in correctly diagnosis the aetiology of nocturia symptoms in your patients.
| Common conditions causing nocturia7,8 | |||
| Overactive bladder (OAB)9–12 | Bladder outlet obstruction (BOO)1,12–16 | Nocturnal polyuria (NP)1,6,12,17,18 | |
| Description | Muscles of bladder start to contract involuntarily even when volume of urine in bladder is low | Blockage to the base of the bladder, reducing or stopping the flow of urine into the urethra | Passing of large volumes of urine at night due to absence of diurnal rhythm of antidiuretic hormone (ADH) system
24-hour urine output is normal or only moderately increased |
| Gender | Female & male | Male > female | Female = male |
| Symptoms | Nocturia, urinary incontinence, urinary urgency, increased frequency of urination, sleep disturbance, fatigue | Abdominal pain, frequent urination, dysuria, hesitancy, poor stream, intermittent stream, terminal dribbling, nocturia, urinary tract infection, sleep disturbance | Nocturia, sleep disturbance |
| Causes | Multifactorial
Specific cause of OAB is still unknown |
Multifactorial Large prevalence due to benign prostatic hyperplasia among men |
Multifactorial
Can be idiopathic |
| Risk factors for development | Elderly patients with cognitive decline | Largely dependent on cause | Largely dependent on cause |
| Diagnosis | Medical history
Physical exam Urine sample Neurological exam Fluid and bladder diary |
Physical exam
Digital rectal exam Blood chemistries Prostate-specific antigen testing Cystoscopy and retrograde urethrogram Uroflowmetry Urodynamic testing Ultrasound Urinalysis / urine culture |
Medical history
3-day bladder diary ADH levels |
| Treatment | Behavioural strategies such as pelvic floor exercises or scheduled toilet trips
Lifestyle modifications such as fluid restriction Anticholinergics Antimuscarinics Bladder injections (e.g. botox) Invasive/non-invasive nerve stimulation Surgery (last resort) |
Largely dependent on cause
Urinary catheterisation Prostate-specific:
|
Largely dependent on cause
Fluid restriction Lifestyle modification ADH analogues (desmopressin) |
Job Code: UK-NOQD-2000015 - Date of preparation: January 2023